Story Highlights
- Heart attack doubles the odds of depression diagnosis
- Link holds after taking demographics into account
WASHINGTON, D.C. -- U.S. adults who have had a heart attack are twice as likely as those who have not had a heart attack to report being diagnosed with depression at some point in their lives, 30.1% vs. 15.0%, respectively.
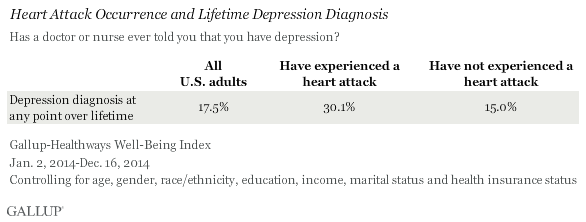
Importantly, the link between heart attacks and depression holds true after controlling for the effects of age, gender, race/ethnicity, education, income, marital status and health insurance status.
Similarly, those who have had a heart attack are twice as likely as those who have not to say they are currently being treated for depression. While 8.1% of those who have never experienced a heart attack currently contend with depression, this figure jumps to 16.5% among those with a history of at least one heart attack.
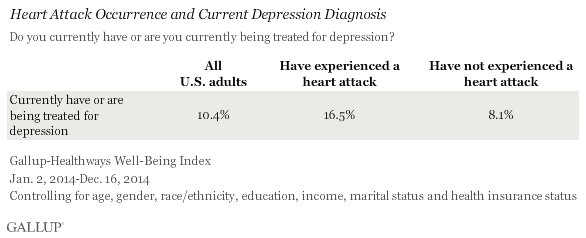
Overall, in data collected from Jan. 2, 2014 through Dec. 16, 2014, 17.5% of Americans report having been diagnosed with depression at some point in their lifetime, and 10.4% currently have depression or are being treated for it. About one out of every 25 U.S. adults (3.8%) report having experienced a heart attack at some point in their lives.
These results are based on interviews with 164,102 adults in the U.S. conducted as part of the Gallup-Healthways Well-Being Index, of which 6,236 report having experienced a heart attack at some point in their lifetime.
Implications
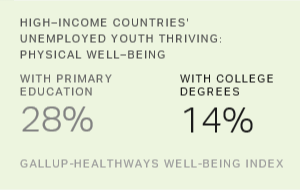
Heart disease and depression are two of the most costly diseases in the U.S. They affect individuals' quality of life and well-being and create an enormous burden on the U.S. healthcare system and economy. Heart disease is the leading cause of death for men and women in the U.S., and the Centers for Disease Control and Prevention estimates that coronary heart disease costs the U.S. $108.9 billion each year in healthcare services, medications and lost productivity. Depression is the leading cause of disability worldwide among all chronic diseases. Previous Gallup research shows that depression costs U.S. employers $23 billion annually in lost productivity, and those who are unemployed, especially the long-term unemployed, are even more likely to be diagnosed with depression.
These results, however, do not prove that heart attacks increase a person's odds of having depression, but they do show that the two are closely linked. Depression is a known predictor of cardiac problems and is as strong a risk factor for heart disease as diabetes and smoking. Studies suggest the relationship between depression and heart disease develops from underlying behavioral and physiological mechanisms related to depression such as a lack of self-care, self-medicating through food or substances and hormonal and inflammatory problems, which trigger heart disease. Consequently, a depression diagnosis could potentially increase the chance of having heart attack, and being obese -- a risk factor for both heart disease and depression -- might simultaneously increase the likelihood of having a heart attack and being diagnosed with depression. Depression diagnoses, therefore, can and do pre-date heart attack occurrence.
Dr. Dean Ornish, founder of the Preventive Medicine Research Institute, explains how symptoms of depression can increase the odds of experiencing a heart attack: "Feeling depressed makes it harder to make healthy lifestyle choices. People are more likely to smoke, overeat, drink too much and work too hard when they're feeling lonely and depressed. One patient said to me, 'I've got 20 friends in this pack of cigarettes, they're always there for me and no one else is -- you want to take away my 20 friends?' In our research, we've found that people are more likely to make lifestyle choices that are life-enhancing than self-destructive when they're feeling happy and loved."
In addition, substantial research suggests the relationship may also point in the other direction: Those who experience a heart attack will be much more likely to be diagnosed with depression later. After all, a heart attack not only affects the cardiac system, but also it can alter an individual's entire life experience, including his or her autonomy, sense of security and confidence in the future, physical capabilities, and ability to resume living a normal life.
Research also suggests the link between heart attack and depression extends to mortality. Researchers at the Montreal Heart Institute found that those who were depressed were six times more likely to die within six months of their heart attack than those who were not depressed.
The psychological aspects of living with illness must be given proper attention in healthcare. Preventing and recovering from a heart attack and subsequent depression often depends on making positive lifestyle choices and having a strong support network. Symptoms of cardiac issues and depression can overlap -- fatigue, disruption of daily routines, sleep disturbance -- so it is vital that caregivers assess and treat heart attack and depression simultaneously. And to decrease the prevalence of these connected conditions, healthcare professionals could recommend lifestyle changes to help treat both of them, thus focusing on the connection between heart attack and depression by caring for the whole person.
Survey Methods
Results are based on telephone interviews conducted Jan. 2, 2014 through Dec. 16, 2014, as part of the Gallup-Healthways Well-Being Index survey, with a random sample of 164,102 adults, aged 18 and older, living in all 50 U.S. states and the District of Columbia. Of these, 6,236 report having experienced a heart attack at some point in their lifetime.
For results based on the respondents reporting having had a heart attack, the margin of sampling error is approximately ±1.1 percentage points at the 95% confidence level. For those who reported never having had a heart attack, the margin of error is ±0.2 percentage points. All reported margins of sampling error include computed design effects to account for the weighting of the data.
Each sample of national adults includes a minimum quota of 50% cellphone respondents and 50% landline respondents, with additional minimum quotas by time zone within region. Landline and cellular telephone numbers are selected using random-digit-dial methods.
Learn more about how the Gallup-Healthways Well-Being Index works.