Story Highlights
- In U.S., 28.0% of adults are obese
- Diabetes rate was 11.4% in 2015, matching all-time high
- Whites show sharpest uptick in obesity and diabetes rates
WASHINGTON, D.C. -- The obesity rate among U.S. adults in 2015 climbed to a new high of 28.0%, up 2.5 percentage points since 2008. This represents an increase of about 6.1 million U.S. adults who are obese.

These results are based on more than 175,000 interviews conducted each year from 2013 to 2015 and more than 350,000 interviews conducted each year from 2008 to 2012 as part of the Gallup-Healthways Well-Being Index. Unlike some government estimates of obesity, the Well-Being Index uses respondents' self-reported height and weight to calculate body mass index (BMI). It does not involve in-home clinical measurements that typically result in higher obesity estimates.
In addition to the 28.0% who are obese, another 35.6% of adults are classified as overweight, with 34.6% normal weight and 1.8% underweight, as reported in 2015.
As with obesity, diabetes generally has trended upward since 2008. The rates of both conditions declined slightly in 2011, only to see annual upticks in the years since. The obesity and diabetes trends typically parallel each other given the close relationship between the two health conditions, but are not always in lockstep. In 2015, 11.4% of Americans reported having been diagnosed with diabetes, unchanged from 2014. This equates to about 27.9 million adults living with diabetes.
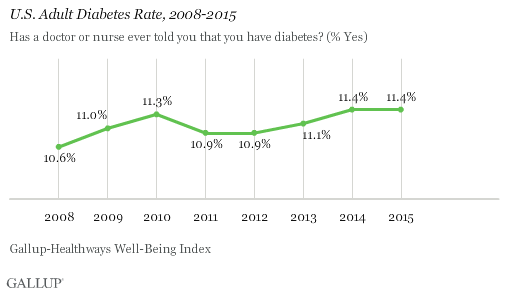
The Well-Being Index does not measure new onset of diabetes, but rather the percentage of adults who report ever having been diagnosed with it in their lifetime. The Well-Being Index does not discern between Type 1 and Type 2 diabetes.
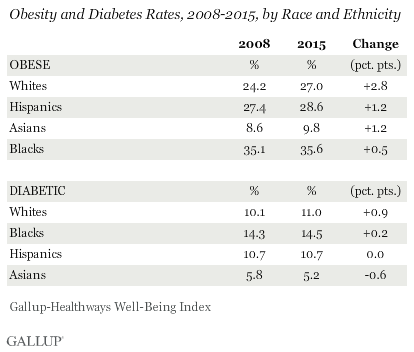
Whites See Sharpest Uptick in Obesity, Diabetes Rates
Across racial and ethnic groups, increases in obesity and diabetes rates since 2008 have been uneven. Both rates have increased much more among whites than among blacks, Asians and Hispanics. Blacks have the highest obesity rate by far of the major racial and ethnic groups, followed by Hispanics, but these two groups have had comparatively modest increases in obesity since 2008, and have shown little to no change in diabetes diagnoses during this time.
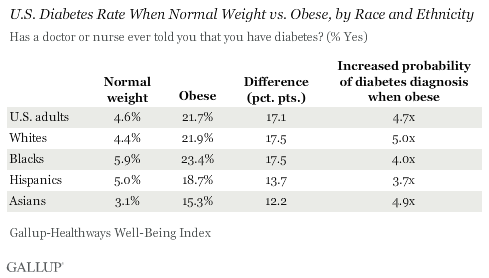
There is a discernible link between obesity and diabetes among both individuals and large populations. The increased probability of a diabetes diagnosis among those who are obese compared with those of normal weight is similar across all major race and ethnic groups, and is thus an equally important health issue regardless of racial or ethnic identity. Overall, adults who are currently obese are about 4.7 times more likely to be diabetic compared with those who are normal weight, a probability that doesn't vary significantly for individual racial or ethnic groups. Diabetes diagnoses can and do occur among normal-weight individuals, though it is much less likely.
Implications
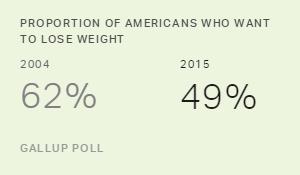
The obesity rate has continued to rise in the U.S. after leveling off from 2011 to 2013, and has done so despite rising public concern. Past research has demonstrated that obesity and its associated chronic conditions including diabetes cost the U.S. economy $153 billion per year in unplanned absenteeism due to poor health, a figure that has increased since the time of that study. And while blacks suffer disproportionately from chronic conditions associated with obesity, the sharp increase in obesity measured among whites since 2008 signifies that this is not a problem isolated to one racial or ethnic group.
Obesity affects all elements of well-being, not just physical wellness. It is associated, for example, with lower financial and social well-being. While obesity can diminish overall well-being, the relationship can also work in reverse; high well-being can reduce the chances of being obese. Those who have high or improving well-being across all five elements -- purpose, social, financial, community and physical -- are less likely to be obese or to become obese in the future than those who do not.
States, communities and workplaces alike can develop interventions targeting the behaviors linked to obesity. While exercise, produce consumption and healthy eating are all important factors, less obvious aspects of poor well-being are also key predictors of its occurrence, including smoking, depression, food insecurity, not having a safe place to exercise, not having a personal doctor and exhibiting poor dental habits. Having an accountability partner who encourages healthy choices and learning new and interesting things daily are also demonstrated deterrents to obesity. It is also important to recognize those occupations that are most at risk for obesity, including transportation, manufacturing/production and installation/repair workers. By addressing obesity on all relevant fronts, it is possible to reverse the upward trend and, in turn, decrease diabetes rates as well.
Survey Methods
Results are based on telephone interviews conducted Jan. 2-Dec. 30 in each year from 2008 through 2015, as part of the Gallup-Healthways Well-Being Index, with a random sample of over 350,000 adults in 2008-2012 and over 175,000 adults in 2013-2015, aged 18 and older, living in all 50 U.S. states and the District of Columbia. For results based on the total sample of national adults, the margin of sampling error is ±0.2 points at the 95% confidence level. The margin of sampling error for the four major race and ethnic groups ranges from ±0.3 points for whites to less than ±2.0 points for Asians. All reported margins of sampling error include computed design effects due to weighting.
For data collected before Sept. 1, 2015, each daily sample of national adults includes a minimum quota of 50% cellphone respondents and 50% landline respondents. For data collected between Sept. 1, 2015, and Dec. 30, 2015, each daily sample of national adults includes a minimum quota of 60% cellphone respondents and 40% landline respondents. Cell proportions have been steadily increased since 2008, when 15% of respondents were interviewed by cell. Additional minimum quotas are by time zone within region.
Learn more about how the Gallup-Healthways Well-Being Index works.